The NHS is fighting to provide safe and effective care for all cancer patients, say leading doctors.
The Royal College of Radiologists is warning that the UK’s four nations are facing “chronic understaffing”, with patients waiting too long for vital tests and treatment.
Half of all cancer units now report frequent delays for both radiotherapy and chemotherapy.
Ministers say a workforce strategy for the NHS in England will be presented shortly.
The plan, which purports to detail how the government will fill staffing gaps over the next 15 years, has repeatedly been delayed, to the frustration of some in the health service.
Elsewhere in the UK, ministers say cancer waiting lists are a priority and additional investment is being made in staff and diagnostic equipment.

Carol Fletcher, 57, from Usk, in south Wales, says she has faced multiple delays in cancer treatment since she was diagnosed last summer.
In June 2022, Carol Fletcher, from South Wales, finally had her routine screening appointment for breast cancer, which was already overdue.
“It was another eight weeks after my mammogram before they told me something was wrong,” she said.
Since her cancer diagnosis, there has been more waiting: scans, tests, surgery, and then chemotherapy.
“They told me I may not get the results (quickly) after my mastectomy because they don’t have enough pathologists, so there was another eight-week delay for chemotherapy,” she said.
“I can’t plan ahead and it has had a huge impact on my family.”
NHS services across the UK have been struggling to meet cancer targets since long before Covid.
The pandemic increased the backlog, with scans and treatments interrupted by lockdowns.
In England, Scotland and Northern Ireland, a key aim is to start treatment within two months of an urgent referral from a GP.
In Wales the measure is slightly different as it includes all non-urgent and urgent referrals.
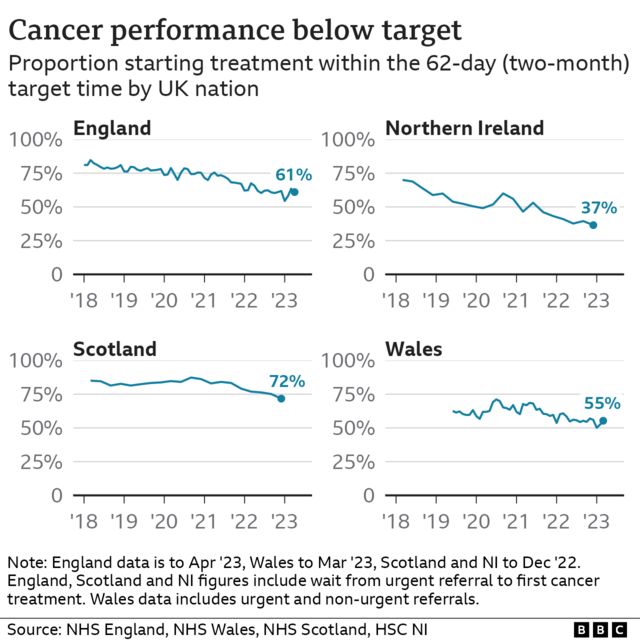
All four nations are operating well below those levels. In England, only 64% of patients start treatment at this time against a target of 85%.
Increasing delays are, in part, the other side of a medical success story.
Scientific progress in cancer care has been remarkable, with next-generation drugs offering hope where little could be done before.
The new techniques are more effective, but often much more complex for clinicians to apply.
At the same time, the UK population is ageing, and since cancer risk is strongly related to age, it means increased demand for expensive scanners, along with more staff to analyze those scans and more specialist doctors and nurses.
The Royal College of Radiologists (RCR) describes the situation as a perfect storm and says the workforce is struggling to keep up.
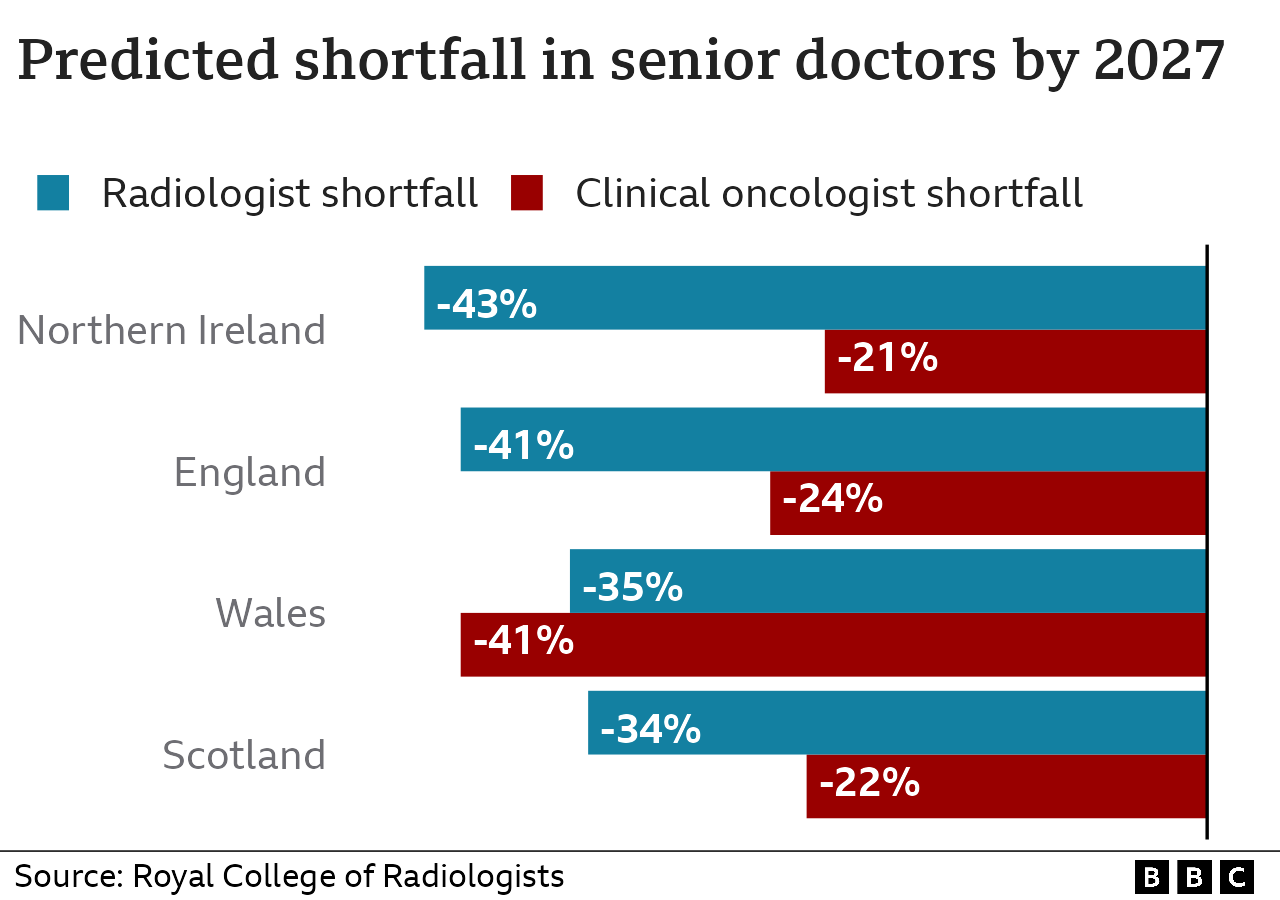
Across the four UK nations, he estimates there is now a 15% shortfall of specialist cancer doctors, or clinical oncologists, delivering chemotherapy and radiotherapy.
Without action, he says this gap will grow to 25%, or a shortage of 368 full-time consultants, by 2027.
Just as worrisome is an even greater shortage of consultant radiologists: highly trained doctors who interpret scans to diagnose cancer or monitor its progression.
‘Perfect storm’
The RCR says that for every month a patient waits to start cancer treatment, the risk of death increases by about 10%.
In their annual survey, 44% of cancer service managers say they are now “very concerned” about patient delays, up from 29% the year before.
“There are examples in almost every cancer center where parts of the service just don’t work as well as we’d like,” said Dr. Tom Roques, consultant oncologist and RCR vice president.
“We have to tell patients all the time that we can’t treat them as fast as we’d like, or in the way we’d like to, and that’s stressful.”

Kevin O’Hara was diagnosed with kidney cancer after a motorcycle accident.
Kevin O’Hara, 60, of County Durham, broke five ribs in a motorcycle accident last November.
A scan of her upper body also detected a shadow near one of her kidneys which was later diagnosed as cancer.
He was offered a drug treatment aimed at slowing the growth of the tumor and, in early February, was told that the waiting list for surgery would be three to four months.
That period is over, but he is still waiting for a date for his operation.
“Every day you’re waiting and waiting and nothing changes,” he said.
“I get home from work and go to the door and when there isn’t an envelope that says NHS on the top, I get really depressed.”
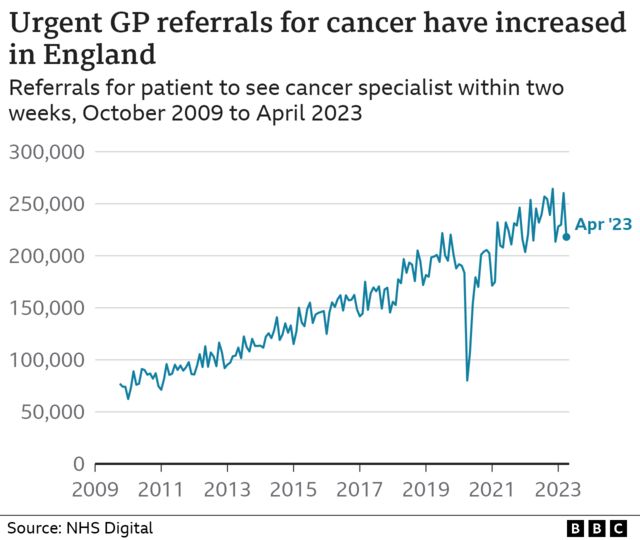
There is another trend in cancer care that is often overlooked.
The reasons for this are complex and include a pick-up in demand since Covid, stronger guidance for GPs to refer to cancer specialists, major NHS ad campaigns and the work of campaigners such as “Bowelbabe” Deborah James.
Oncologists call the increased demand a “very good thing” as an increasing proportion of patients are now being diagnosed earlier, when cancer is easier to treat.
But it also puts more pressure on NHS services, as waiting times for diagnosis and other examinations are one of the key bottlenecks in the system.
The RCR also says there is a “breath of light”, with oncologist hiring increasing in the last three years, particularly in the parts of the country with the worst staff shortages.
He wants every UK nation to increase medical school places and training positions, and says more must also be done to prevent experienced staff cutting back on hours or leaving the profession early.
The Department of Health said the total number of full-time staff in the cancer workforce in England increased by 51% to 33,093 since 2010.
A spokesperson added: “We want to build on this progress and will be publishing a workforce plan shortly to ensure we have the right number of staff, with the right number of skills.”
The Scottish government is also expected to publish its new 10-year cancer strategy in a matter of weeks, establish ways to attract and retain more staff.
The Welsh government recently published a cancer improvement plan and says it is now investing heavily to train more staff and build more diagnostic and treatment centers.
In Northern Ireland, the health department said it was “extremely disappointing” that cancer targets were not being met. has recently opened two new rapid diagnostic centers and began a “cancer strategy workforce review.”
Data visualization by Liana Bravo.

